COVID-19 Pandemic and Mental Well-Being: A Study Conducted on Medical Students and Their Parents in a Private Medical College in Pakistan
by Misha Khan * ![]()
![]() , Mufliha Ibrahim
, Mufliha Ibrahim![]() , Muhammad Saad Shabbir
, Muhammad Saad Shabbir ![]() , Muhammad Huzaifa Tofique, Muhammad Naheel Khalili, Muhammad Asad, Muhammad Ahmed, Muhammad Haroon, Saima Zainab
, Muhammad Huzaifa Tofique, Muhammad Naheel Khalili, Muhammad Asad, Muhammad Ahmed, Muhammad Haroon, Saima Zainab
Liaquat National Hospital and Medical College, Karachi, Pakistan
* Author to whom correspondence should be addressed.
Journal of Engineering Research and Sciences, Volume 2, Issue 2, Page # 1-7, 2023; DOI: 10.55708/js0202001
Keywords: Covid-19, pandemic, coronavirus, mental well-being, parents, medical students, MBBS students
Received: 24 November 2022, Revised: 21 January 2023, Accepted: 25 January 2023, Published Online: 22 February 2023
APA Style
Khan, M., Ibrahim, M., Shabbir, M. S., Tofique, M. H., Khalili, M. N., Asad, M., Ahmed, M., Haroon, M., & Zainab, S. (2023). COVID-19 Pandemic and Mental Well-Being: A Study Conducted on Medical Students and Their Parents in a Private Medical College in Pakistan. Journal of Engineering Research and Sciences, 2(2), 1–7. https://doi.org/10.55708/js0202001
Chicago/Turabian Style
Khan, Misha, Mufliha Ibrahim, Muhammad Saad Shabbir, Muhammad Huzaifa Tofique, Muhammad Naheel Khalili, Muhammad Asad, Muhammad Ahmed, Muhammad Haroon, and Saima Zainab. “COVID-19 Pandemic and Mental Well-Being: A Study Conducted on Medical Students and Their Parents in a Private Medical College in Pakistan.” Journal of Engineering Research and Sciences 2, no. 2 (February 1, 2023): 1–7. https://doi.org/10.55708/js0202001.
IEEE Style
M. Khan et al., “COVID-19 Pandemic and Mental Well-Being: A Study Conducted on Medical Students and Their Parents in a Private Medical College in Pakistan,” Journal of Engineering Research and Sciences, vol. 2, no. 2, pp. 1–7, Feb. 2023, doi: 10.55708/js0202001.
Pandemics always have a significant effect on the physical, mental, and financial status of people in general. With new variants of coronavirus emerging now and then, it is difficult to process the sudden changes and new healthcare implementations for all individuals. In this situation, our objective was to assess the mental-wellbeing of medical students and their parents and highlight factors that could be associated with their mental-wellbeing deterioration. This is a cross-sectional study in which the non-probability consecutive sampling technique was used. Our sample size was 219 for each population (i.e., parents and medical students). Two questionnaires were designed, one for parents and another for students, each consisting of a personal information section (including personal data and COVID-related questions) and a mental well-being assessing section with the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS). Descriptive data analysis and all calculations are done using SPSS version 22. A total of 438 responses indicates that 35.2% (n = 154) of respondents have probable depression, 14.6% (n = 64) have possible depression, 43.8% (n = 192) have average mental well-being, and only 6.4% (n = 28) have high mental well-being. A comparison of scores for both groups show that the majority of students (44.7%) have probable depression, while most parents (43.8%) have average mental well-being. High mental well-being was found only in 3.2℅ medical students and 9.2℅ of their parents. Hence, the realization of the effects of different factors, including coronavirus, on both groups is essential.
1. Introduction
Pandemics always take a toll on people’s physical health. They are also seen to have significant psychological impacts [1], and the COVID-19 pandemic is no different. Due to its highly contagious nature, it has been advised to limit as much social interaction as possible. Therefore, the lockdown was implemented in various countries, and it has proved quite effective in reducing the number of new COVID-19 cases [2].
The first case of coronavirus in Pakistan was reported from Karachi on February 26, 2020, which eventually led to the implementation of a lockdown in Pakistan on March 13, 2020, by closing borders and educational institutes in the initial phase that was followed by a complete lockdown in multiple cities, forcing the general population to confine themselves to their homes. Although the lockdown was supposed to be lifted in a month due to the degrading conditions, it kept on delaying. On August 9, 2021, the lockdown was eased, but still, there are many restrictions in the state, like fixed business hours, only vaccinated citizens being allowed in public places, 50% attendance of staff in offices, students in institutions, etc.
This pandemic has shaken the global health and economic systems to their core. Almost 800 million people have been pushed down the line of poverty, with nearly 3.3 billion people at risk of losing their livelihoods [3].
With people losing their jobs and children studying from home due to the lockdown, parents and students faced a dilemma. Although being in lockdown would naturally mean parents had more time with the kids, with no end to this situation in sight, the household environment got stressful. As was proved by a longitudinal, observational study conducted in the United States, parent stress increased substantially during COVID-19 and has not returned to its pre-COVID-19 level [4]. It was also recognized in a cross-sectional study done at the University of Wisconsin-Madison and the University of Southern California that 39.4% of parents reported moderate to severe anxiety and/or depression symptoms. Most of these parents testified that their current emotions or concerns interfered with their ability to parent. These effects were more profound in females and low-income families [5].
The COVID-19 outbreak also negatively affected the mental well-being of medical students. An observational study conducted in the Department of Physiology, College of Medicine, King Saud University shows that 56.2% of students suffered academically, 44.1% showed emotional detachment from family and friends, and 23.5% were disheartened [6]. Also, in an online survey in Jordan, about 58.4% of medical students seemed concerned about the inability to get clinical sessions and labs [7]. Likewise, the results of a survey in Australia show that the mental well-being of 68% of medical students declined during COVID-19 [8].
Parents and medical students living in Pakistan, a developing country, cannot be put in the same category as parents and students from other nations, as Pakistan’s government couldn’t support the families as much as governments in developed countries did. Moreover, the median household income for a family living in Pakistan is $508.977, compared to $9,733 [9,10] in the rest of the world. The average family size in Pakistan is 6.7, as compared to the rest of the world, which is 4.9 [11,12]. Also, extended family systems are very common in Pakistan.
A parent is the caretaker of a child. Their main role is to provide for and nurture their children in the best possible manner. The COVID-19 situation took its toll on this role, thus putting stress on parents. Research conducted in Italy showed that 17 percent of the sample collected experienced significant parenting-related exhaustion during the COVID-19 outbreak [13]. In 2017, a research paper highlighted the evidence of the association of stress with ineffective parenting and poor child adjustment [14]. In another study, over-reactive parents, who showed constant expressions of anger and arguing, led to children expressing similar personality traits as their parents [15]. Hence, the well-being of parents has a direct role in the proper upbringing and welfare of the children [16,17]
Moreover, as shown in the results of the study conducted in US medical schools [18], more than 20 percent of the students are considering a shift in their field of specialization after the COVID-19 pandemic, mostly due to the shift in financial status and mental well-being in their household. Therefore, along with parents, it is important to find out the effects this pandemic has had on medical students as well.
The COVID-19 pandemic has caused significant damage to different aspects of society. Even though it affected everyone equally, the influence of this pandemic on parents and medical students has been mostly overlooked. The purpose of this research is to take into consideration parents’ and medical students’ mental well-being during the COVID-19 pandemic. So that positive steps can be taken to ensure a better quality of life for both parents and students.
2. Materials and methods
2.1. Study design, sampling technique, and participants
This is a cross-sectional study in which a non-probability consecutive sampling technique was used. All medical students and their parents were included in this study, except students or parents who have any diagnosed psychological disorder, whether on medications or not. Prior consent was obtained from all participants. No harm or benefit was subjected to any participant. The anonymity of every participant and the confidentiality of their data was ensured.
2.2. Sample size
The sample size was calculated for two independent population proportions using the online sample size calculator “clincal.com” [19]. Using the proportion of increased stress after children’s return to school during COVID-19 among population 1 (parents) as 55% [4] and deterioration of mental well-being during COVID-19 among population 2 (medical students) as 68% [8], the margin of error is 5%, the confidence level is 95%, and the power is 80%. The final sample size calculated is at least 219 in each group.
2.3. Data collection procedure
For 2 years, on and off, the lockdown was implemented, and data was physically collected between February 2022 and June 2022, during new waves of omicron and delta variants of coronavirus. In this survey, physical data were collected from 219 medical students (n1) and their parents (n2). A total of 470 (N) forms were received, 219 from students and 251 from their parents, of which 32 were excluded due to incomplete data or diagnosed psychological disorders. Before participation, consent forms were signed by all participants. Questionnaires were distributed among students from the first year to the final year of medical school, one for the students and two for their parents, which were then filled out individually by all participants and returned to us.
2.4. Instrument
Our team designed a questionnaire consisting of a section containing demographic or personal information, in which COVID-related questions were also included, and a section assessing mental well-being with the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS), a 14-item scale. The scoring range for each item was from 1–5, and the total score is from 14–70. This provided a WEMWBS cut point of 40 or less for probable depression, 41–44 for possible depression, 45–59 for average mental well-being, and scores of 60 or more for high mental well-being.
2.5. Data analysis
Descriptive data analysis and all calculations were done using SPSS version 22. The mean and standard deviation were calculated for continuous variables like age, family size, and WEMWBS scores. Frequency and percentage were calculated for categorical variables like gender, marital status, employment status, and monthly income. By applying Chi-square and Fischer exact tests, the association between qualitative variables was determined. An independent t-test was used to find the mean difference between the WEMWBS scores of both groups. A p-value of <0.05 will be considered significant.
3. Results
3.1. Report of parents’ responses:
The results of the response show a contribution of 54.8% males and 45.2% females, with a mean age of 51.54 years. Most respondents belong to the nuclear family type (71.7%), and 13.2% of them are single parents. Variations were found in the answers to the question of employment status: 56.6% were employed, 36.1% were homemakers (mostly females), 1.4% chose the category of others, and 5.9% were unemployed. The majority of the participants were of high socioeconomic status (65.4℅) and owned their homes (83.6 %). Parents usually had no (43.4%) or one (42.9%) comorbidity. Family COVID positivity was reported at 56.6%, whereas 32.4% of them tested positive for COVID. 28.8% of them lost their close ones to COVID. Their WEMWBS mean score was 47.21. In parents, the probable depression was 25.6%, the possible depression was 13.2%, the average mental well-being was 51.6%, and the high mental well-being was 9.6%. (Table 1).
3.2. Report of Students’ responses
Students taking part in this survey were 68℅ females and 32% male with a mean age of 20.69 years. Responses comprise 38.8℅ from the third year of medical school, 33.2% from the second year, 12.8% from the fourth year, 7.8% from the first year, and 7.3℅ from the final year, with an average GPA of 3.08 (SD = 0.398) across all years. Hostilities were 21.5℅ while the rest of the participants were day scholars. Similar to their parents’ results, the majority live in a nuclear family system (74%) and come from a high socioeconomic class (81.5%). About 64.8% of students reported a decrease in study hours, 16.9% reported an increase in their study hours, and 18.3% reported that their study hours remained unchanged. Across all five years, the mean WEMWBS score was 41.68. In students, probable depression was scrutinized at 44.7%, possible depression at 16.0%, average mental well-being at 36.1%, and high mental well-being at 3.2% (Table 1)
3.3. Comparison of Parents’ and Students’ Mental – well-being
An independent t-test was applied to compare the means of parents’ and students’ WEMWBS scores, and the mean difference was found to be statistically significant (p<0.001). The mean difference can also be seen in Figure 1. A Pearson chi-square test was used to determine if there was a significant relationship between parents’ and students’ well-being, and the results were highly significant(0.001).

Figure 1: Box and whisker plots showing variation in the WEMWBS scores of students and parents.
Table 1: Responses of parents and students and their corresponding p-values
Parents n (%) | Students n (%) | P-value | ||
Gender | Male | 120 (54.8) | 70 (32) | <0.001 |
Female | 99(45.2) | 149 (68) | ||
Age | Mean ±SD | 51.54 ±6.766 | 20.69 ±1.228 | <0.001 |
Family type | Nuclear | 157(71.7) | 162 (74) | 0.591 |
Extended | 62(28.3) | 57 (26) | ||
Household income | Under Rs. 25000 | 6 (3.4) | 0 (0) | <0.001 |
Between Rs.25,000 – Rs.50,000 | 7 (3.9) | 4 (2.2) | ||
Between Rs.50,000 – Rs.75,000 | 18 (10.1) | 3 (1.7) | ||
Between Rs.75,000- Rs.1,00,000 | 31 (17.3) | 26 (14.6) | ||
Rs.1,00,000 or over | 117 (65.4) | 145 (81.5) | ||
Family tested positive for covid | Yes | 124 (56.6) | 140 (63.9) | 0.118 |
No | 95 (43.4) | 79 (36.1) | ||
Deaths by covid | Yes | 63 (28.8) | 52 (23.7) | 0.232 |
No | 156 (71.2) | 167 (76.3) | ||
Tested positive for covid | Yes | 71 (32.4) | 61 (27.9) | 0.289 |
No | 148 (67.6) | 158 (72.1) | ||
WEMWBS score | Mean ±SD | 47.21 ±9.839 | 41.68 ±9.684 | <0.001 |
Mental Well-being | Probable depression | 56 (25.6) | 98 (44.7) | <0.001 |
Possible depression | 29 (13.2) | 35(16) | ||
Average mental well-being | 113 (51.6) | 79 (36.1) | ||
High mental well-being | 21 (9.6) | 7 (3.2) | ||
4. Discussion
The COVID-19 pandemic was a time of intense uncertainty, fear, and stress, and its effects were seen in both groups’ mental well-being, which was found to be on the lower end of the spectrum, more in students than in parents. Through an independent sample t-test, the mean difference between the WEMWBS scores of participants who had tested positive for COVID-19 during the pandemic and those who didn’t were found to be significant (p=0.019) which points to the possibility that they might still be suffering from the after-effects of being quarantined or be on their path to recovery. Using the Pearson chi-square test, no significant relationship was found between participants’ mental well-being status in nuclear and extended family systems (p = 0.845).
Results of this study show that students who are suffering from probable depression are 44.7%, which is alarmingly high; however, one thing that stood out in the results of this study was that the students of different years had different levels of mental well-being (Figure 2). Second and fourth-year students had the best mental health, which can be attributed in part to the fact that second-year students had already been exposed to the medical world in their first year, so they knew what steps to take to perform well. Similarly, fourth-year students also became familiar with their clinical rotation schedule, due to which they reported relatively higher mental well-being despite the pandemic. The study conducted on medical students in Australia [8] showed somewhat similar results: first-year students showed the highest level of distress, with 24% of first-year students scoring ‘very high’ The third year showed surprisingly lower rates of distress, with only 9% of students scoring in the ‘very high’ category, as compared to 44.7% of students showing probable depression in this study. These findings on student mental well-being are important to address, as poor mental health in medical students may make them less enthusiastic physicians in the future, which will ultimately affect the delivery of healthcare services in the country. Medical colleges should organize regular group sessions to keep their students’ mental health in check. In a study done in Canada, it was found that participation in extracurricular activities or school sports was associated with better mental health outcomes in children and youth [20]. This emphasizes the importance of being proactive in hobbies where a student finds peace and thoroughly enjoys himself/herself while partaking in those activities, whether extracurriculars or book reading, for example. PMC should construct some sort of course in their curriculum where the students can easily relieve themselves from the intensely high-paced and competitive environment that medical colleges are known to have.
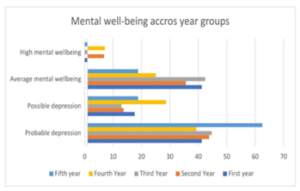
Figure 2: Graph comparing percentages of mental well-being across all year groups
Although the majority of the parents were found to have average mental well-being, a large proportion of parents had probable depression at 25.6% and high mental well-being was only seen in 9% of the parental population, which is worrying and calls for action. If we were to compare these results to the study done on parents in Richmond, US [4], we would find that only 22.4% of parents showed positive results for high stress; this had increased from 3.5%, which was reported before the pandemic. This can be because in Pakistan there are a greater number of people living in joint families as compared to America, where they have nuclear family systems, so added family members tend to increase stress levels. It was also noted that 46.9% of the single parents had probable depression and 18.8% had possible depression, as compared to the proportions of 21.9% and 12.3%, respectively, in non-single parents. The mean difference between the WEMWBS scores of single and non-single parents was also found to be significant (p = 0.002) when an independent sample t-test was applied. This finding can be supported by a study conducted on single parents, which proved that single parents have a higher prevalence of poor mental health compared to partnered parents [21]. Single parents were affected more than parents who were not single. This may be the case because single parents must have faced the socioeconomic burden alone without the financial and emotional support of a partner, thus making them more vulnerable to declining mental well-being. A significant mean difference was also found between the WEMWBS scores of parents with comorbidities and those who didn’t (p<0.001). Moreover, in Pakistan, there is a lack of family security, political unrest, and a poor standard of living. All of these factors combine to cause a disproportionate amount of stress in a Pakistani parent.
According to UNICEF, the good mental well-being of caregivers, whether they’re parents or anyone else, is key to thriving families [22]. and thus, they must have high mental well-being. Promotion of family counseling through mass media should be done to improve family resilience both before and during any crisis such as this pandemic. Moreover, institutions should regularly invite parents to seminars and make them aware of the importance of mental well-being through the statistical data provided in this study.
Limitations include the cross-sectional study design, self-reported questionnaires by students on behalf of parents, and higher female students’ participation. Also, there was a slight difference in the reporting of socioeconomic status by parents and their children, which we assume means that their children do not know about their monthly household income or that many people went into financial losses during COVID that their children do not know about.
5. Conclusions
In a nutshell, this study shows highly significant results. Students’ well-being was seen to be most affected by the coronavirus, whereas parents’ mental well-being was average. As these groups are highly vulnerable to depression, creating awareness about their mental health is crucial, especially during this time. We hope that the sensitivity of this issue will be understood and that together we will bring about a positive change.
List of Abbreviations
COVID-19 (coronavirus disease of 2019), MBBS (Bachelor of Medicine, Bachelor of Surgery), WEMWBS (Warwick- Edinburgh Mental Well-being Scale).
Conflict of Interest
The authors declare no conflict of interest.
Funding Source:
The authors received no financial support for the research, authorship, and publication of this article.
- D. Cuadra-Martínez, P.J. Castro-Carrasco, J. Sandoval-Díaz, D. Pérez-Zapata, D. Mora Dabancens, “COVID-19 y comportamiento psicológico: revisión sistemática de los efectos psicológicos de las pandemias del siglo XXI [COVID-19 and psychological behavior: a systematic review of the psychological effects of 21st century pandemics],” Revista Médica de Chile, vol. 148, no. 8, pp. 1139–1154, 2020, doi:10.4067/S0034-98872020000801139.
- V. Alfano, S. Ercolano, “The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis,” Applied Health Economics and Health Policy, vol. 18, no. 4, pp. 509–517, 2020, doi:10.1007/s40258-020-00596-3.
- World Health Organization, Impact of COVID-19 on people’s livelihoods, their health and our food systems, https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people’s-livelihoods-their-health-and-our-food-systems, 2020.
- E.L. Adams, D. Smith, L.J. Caccavale, M.K. Bean, “Parents Are Stressed! Patterns of Parent Stress Across COVID-19,” Frontiers in Psychiatry, vol. 12, , 2021, doi:10.3389/fpsyt.2021.626456.
- M.L. Kerr, H.F. Rasmussen, K.A. Fanning, S.M. Braaten, “Parenting During <scp>COVID</scp> ‐19: A Study of Parents’ Experiences Across Gender and Income Levels,” Family Relations, vol. 70, no. 5, pp. 1327–1342, 2021, doi:10.1111/fare.12571.
- S.A. Meo, D.A.A. Abukhalaf, A.A. Alomar, K. Sattar, D.C. Klonoff, “COVID-19 Pandemic: Impact of Quarantine on Medical Students’ Mental Wellbeing and Learning Behaviors,” Pakistan Journal of Medical Sciences, vol. 36, no. COVID19-S4, 2020, doi:10.12669/pjms.36.COVID19-S4.2809.
- K. Seetan, M. Al-Zubi, Y. Rubbai, M. Athamneh, A. Khamees, T. Radaideh, “Impact of COVID-19 on medical students’ mental wellbeing in Jordan,” PLOS ONE, vol. 16, no. 6, pp. e0253295, 2021, doi:10.1371/journal.pone.0253295.
- Z. Lyons, H. Wilcox, L. Leung, O. Dearsley, “COVID-19 and the mental well-being of Australian medical students: impact, concerns and coping strategies used,” Australasian Psychiatry, vol. 28, no. 6, pp. 649–652, 2020, doi:10.1177/1039856220947945.
- CEIC, Pakistan Household Income per Capita 2005-2019, https://www.ceicdata.com/en/indicator/pakistan/annual-household-income-per-capita, 2019.
- G. Phelps, S. Crabtree, Worldwide, Median Household Income About $10,000, 2013.
- National Institute of Population Studies-NIPS, Pakistan Maternal Mortality Survey, Islamabad/Pakistan, 2020.
- S. Kramer, With billions confined to their homes worldwide, which living arrangements are most common? https://www.pewresearch.org/fact-tank/2020/03/31/with-billions-confined-to-their-homes-worldwide-which-living-arrangements-are-most-common/, 2020.
- M. Spinelli, F. Lionetti, M. Pastore, M. Fasolo, “Parents’ Stress and Children’s Psychological Problems in Families Facing the COVID-19 Outbreak in Italy,” Frontiers in Psychology, vol. 11, 2020, doi:10.3389/fpsyg.2020.01713.
- M.E. McQuillan, J.E. Bates, Parental Stress and Child Temperament, Springer International Publishing, Cham: 75–106, 2017, doi:10.1007/978-3-319-55376-4_4.
- P. Prinzie, C.M. van der Sluis, A.D. de Haan, M. Deković, “The Mediational Role of Parenting on the Longitudinal Relation Between Child Personality and Externalizing Behavior,” Journal of Personality, pp. no-no, 2010, doi:10.1111/j.1467-6494.2010.00651.x.
- S.B. Wolicki, R.H. Bitsko, R.A. Cree, M.L. Danielson, J.Y. Ko, L. Warner, L.R. Robinson, “Mental Health of Parents and Primary Caregivers by Sex and Associated Child Health Indicators,” Adversity and Resilience Science, vol. 2, no. 2, pp. 125–139, 2021, doi:10.1007/s42844-021-00037-7.
- Centers for Disease Control and Prevention (CDC), Mental health of children and parents —a strong connection, https://www.cdc.gov/childrensmentalhealth/features/mental-health-children-and-parents.html#:~:text=The%20mental%20health%20of%20children,support%20their%20children’s%20mental%20health, 2021.
- Y.M. Byrnes, A.M. Civantos, B.C. Go, T.L. McWilliams, K. Rajasekaran, “Effect of the COVID-19 pandemic on medical student career perceptions: a national survey study,” Medical Education Online, vol. 25, no. 1, 2020, doi:10.1080/10872981.2020.1798088.
- Clincal.com, Sample Size Calculator (online), https://clincalc.com/Stats/SampleSize.aspx, Nov. 2021.
- K. LaForge-MacKenzie, K. Tombeau Cost, K.C. Tsujimoto, J. Crosbie, A. Charach, E. Anagnostou, C.S. Birken, S. Monga, E. Kelley, C.L. Burton, R. Nicolson, S. Georgiades, D.J. Korczak, “Participating in extracurricular activities and school sports during the COVID-19 pandemic: Associations with child and youth mental health,” Frontiers in Sports and Active Living, vol. 4, 2022, doi:10.3389/fspor.2022.936041.
- K.A. Kong, H.Y. Choi, S.I. Kim, “Mental health among single and partnered parents in South Korea,” PLOS ONE, vol. 12, no. 8, pp. e0182943, 2017, doi:10.1371/journal.pone.0182943.
- S. Friedlander, B. Perks, Caregiver mental health and well-being: The key to thriving families, https://www.unicef.org/blog/caregiver-mental-health-well-being-key-thriving-families, 2022.

